Pathology
Pathology is the examination of tissues and body fluids in order to make a diagnosis.
This involves taking a tissue sample of the tumor when a biopsy or surgery is done to remove the tumor. The sample is then sent to a pathologist for review. Once the diagnostic lab report is completed, it is sent to your doctor who shares it with you.
Ependymoma is less common than other brain or spinal cord tumors. In addition, it is sometimes difficult to distinguish it from other tumor types. This can make it difficult to diagnose or a delay may occur. Seeking a second opinion is always a good option when dealing with rare diseases. Contact us if you would like a second opinion.
What is the classification system for ependymomas?
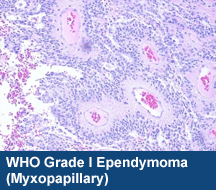
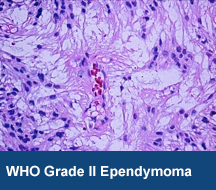
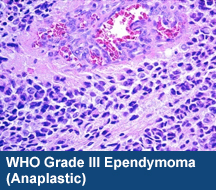
The most widely used system to classify primary brain tumors is the World Health Organization (WHO) system. The WHO uses morphological features to classify these tumors into various ‘types’ and “grades”. This involves examining tissue under a microscope. The WHO was updated in 2016 and again in 2021. In addition to what the tumor looks like under the microscope, molecular changes in the tumor are used to further refine the diagnosis in terms of tumor type and grade.
Unlike other cancers, primary brain and spine tumors generally do not spread (metastasize) outside of the central nervous system (CNS). For this reason, the Tumor-Node-Metastasis (TNM) staging system widely used for most “solid tumor” cancers is not useful for primary brain tumors.
What is classification based on?
The WHO assigns a grade to ependymomas based on the following characteristics:
- Variability in size and shape of the tumor cells (pleomorphism)
- How fast the tumor cells are growing (mitotic count)
- Crowding of tumor cells (cellularity)
- Growth of tumor blood vessels (vascular proliferation)
- Tendency for tumor cells to outgrow their blood supply (tumor necrosis)
- How much the tumor has spread into the surrounding normal tissue (invasion)
- Molecular and genetic features
These criteria apply to both pediatric and adult ependymomas. While a tumor may show characteristics from one or more tumor types and grades, doctors treat patients based on the highest-level tumor grade or what the features are for the majority of the tumor. Visit our treatment section for more details.
What are the types of ependymoma classification?
The WHO classification defines ependymoma and divides them into subtypes.
Subtypes that have been previously recognized by the WHO classification include subependymoma, myxopapillary ependymoma, as well as morphologic variants (for example: cellular ependymoma, papillary ependymoma and tancytic ependymoma).
It is recognized that myxopapillary tumors tend to occur in the spine and subependymomas tend to occur along the ventricles.
Recently, underlying genetic changes have revealed that ependymoma tumor subtypes may be different based on location. There are three locations thought to be important: those that are supratentorial, infratentorial in the posterior fossa, and those located in the spine. Recently, it was discovered that in approximately two-thirds of ependymomas in the supratentorial region, there is a molecular abnormality which is a gene fusion called RELA that results in a unique protein.
This fusion, RELA, results in the uncontrolled activation of a specific tumor cell molecular pathway called the NF-kB pathway. NF-kB contributes to the formation of the tumor and its uncontrolled growth. The 2016 WHO classification recognizes that tumors that are RELA-fusion positive occur in the supratentorial region. If tumors are in the supratentorial region, it is recommend that the tumor is tested for the RELA-fusion protein. The 2021 WHO classification further refined ependymoma molecular pathology. Tumors previously known as ST-RELA ependymoma are now called ST-ZFTA ependymoma and a new classification has been added for of a rare but aggressive spinal tumor: SP-MYCN ependymoma. Read more about the 2021 WHO ependymoma updates.
Scientists are beginning to identify characteristic changes in posterior fossa tumors, and specific epigenetic and gene expression profiles have been identified as potential markers to separate posterior fossa ependymomas into clinically distinct groups.
Finally, myxopapillary and subependymoma continue to be classified based on characteristics seen under the microscope.
It’s important to know your tumor subtype, if available, in order to plan treatment and determine prognosis. Ask your physician if your tumor has subtypes and how your tissue can be evaluated.
The WHO classifies ependymomas into three grades:
Grade I – Subependymoma
Grade II – Myxopapillary Ependymoma and Ependymoma (conventional/classic)
Grade III – Ependymoma (which is the more agressive, previously called anaplastic)
What are the characteristics of each type?
WHO Grade I – Subependymoma
- Slow growing noninvasive tumor
- Are less cellular masses usually attached to the ventricle wall (cerebrospinal fluid filled cavity in the brain).
- More common in adults and older men
- Associated with long-term survival
- Surgery can be potentially curative
WHO Grade II – Myxopapillary Ependymoma
- Slow growing
- Commonly occurs in young adults in the spinal cord, sometimes in the bottom of the spinal cord, an area referred to as “cauda equina”.
- Tend to have good long-term survival after surgical resection
WHO Grade II – Ependymoma (conventional/classic)
- Most common brain tumor in young children
- Most common type of spinal glioma in adults
- Often develop in the ventricles when intracranial
- Several variants exist making diagnosis challenging:
- Cellular ependymoma
- Papillary ependymoma
- Tanycytic ependymoma
- Supratentorial ependymomas can be further subclassified as RELA-positive or RELA-negative (or ZFTA)
- Can potentially recur as a higher grade tumor even after treatment
WHO Grade III - Ependymoma (previously known as anaplastic)
- Show evidence of increased tumor cell growth compared to conventional ependymoma
- Show evidence of new blood vessel formation to support active growth
- Exhibit more aggressive behavior than low grade ependymomas
- Often require additional treatment after surgery and can recur
The relevance of conventional grading (grade II versus grade III ependymomas) and the prognostic relevance of this approach is currently a matter of discussion and debate. Researchers are currently looking at how to better define the features that set apart a grade II from a grade III tumor.
